70 year old female presenting with fever and abdominal pain
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan. is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
CHIEF COMPLAINTS:-





Lower back pain since 2 days
Low grade fever since 10 days
HISTORY OF PRESENTING ILLNESS:-
Patient was apparently asymptomatic 20 years ago. Developed giddiness and which was diagnosed with hypertension and then started on Tab Atenolol.
The patient came to our causality 4 years ago with pain in right hip and she was unable to walk due to a fall from an auto following which she was was diagnosed with right femur fracture and operated in our hospital. Proximal femoral nail was used for fixation.
3 1/2 years ago she developed bleeding with white discharge per vagina and came to OBG department for checkup. She was diagnosed with carcinoma of cervix II B and she underwent radiotherapy at MNJ for 5 weeks in November to December 2019 a total of 25 sessions.
On 7th she developed abdominal pain in the left upper quadrant, which was relieved on vomiting. The vomiting occurs a few hours after eating. The vomit consisted of the food she consumed which is not foul smelling or blood stained and non bilious. She was diagnosed with acid peptic disease. On investigation she was diagnosed incidentally with severe anemia with a haemoglobin of 4gm/dl for which she had blood transfusion on 11th November and she was discharged on 16th November. Investigations also relieved pernicious anemia.
On 23rd November , she came to opd with lower back pain since 2 days, associated with fever since 1 week. The pain is continuous, dull aching type, radiating to groin, no tenderness, no history of tingling or numbness. There are no aggravating factors and the pain is temporarily relieved on medication.
The fever is insidious in onset, gradually progressive, associated with 3 episodes of nausea and vomiting
TREATMENT HISTORY:-
Tab. Atenolol for hypertension.
Chemo radiation 4 years ago for 5 weeks for the treatment of Cervical carcinoma stage IIB.
She had blood transfusion for severe anemia ( hb 4 gm%)
GENERAL EXAMINATION:-
Patient is conscious, coherent, uncooperative
Well oriented to time, place and person
Thinly built and moderately nourishment.
VITALS :-
Temp - afebrile
BP - 130/90 mm/hg
PR - 86 bpm
RR - 13 cpm
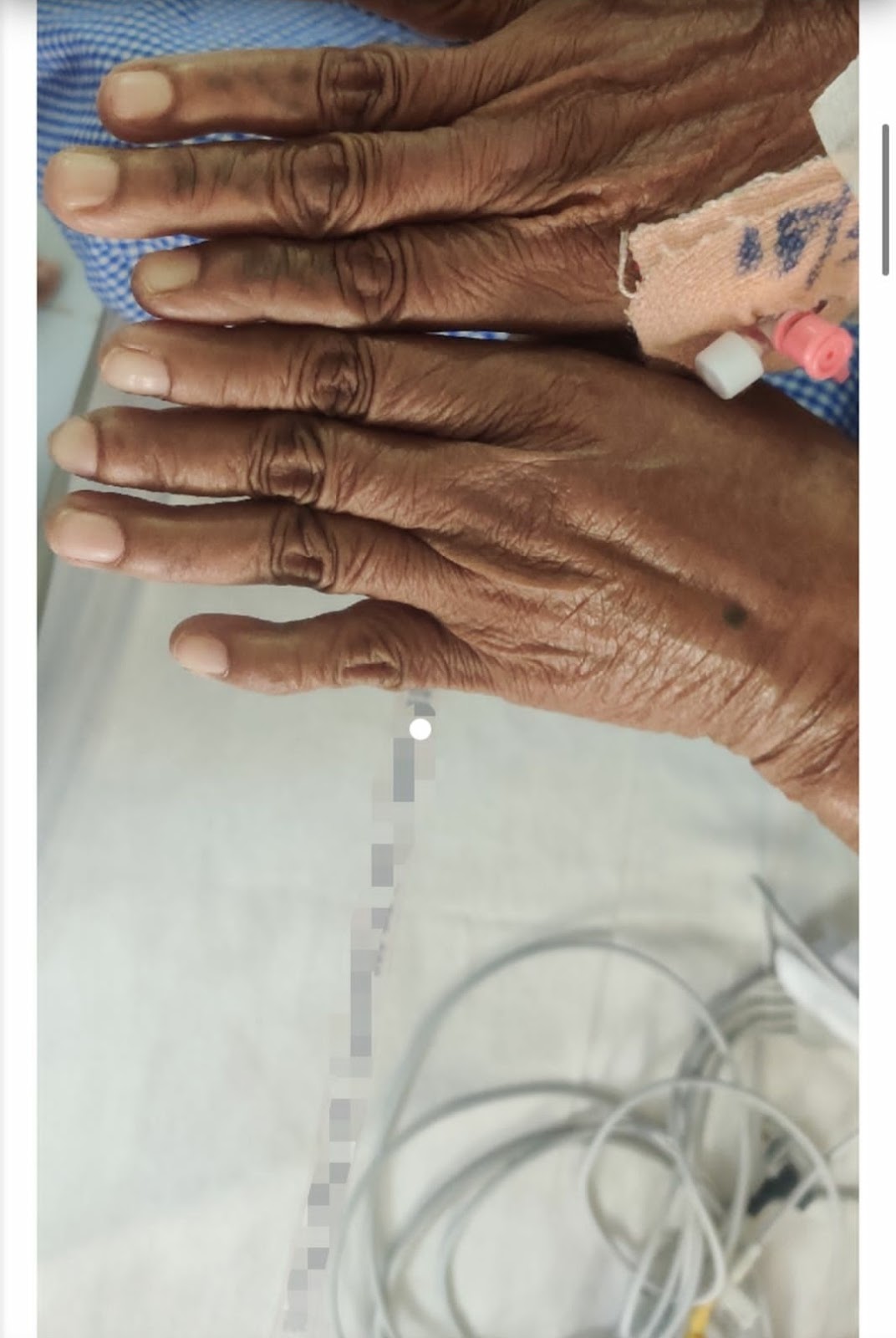
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - absent
Pedal edema - absent
SYSTEMIC EXAMINATION:
CVS
S1 S2 heard
Murmur heard in aortic area.
RESPIRATORY
Chest bilaterally symmetrical, all quadrants
moves equally with respiration.
Trachea central, chest expansion normal.
Resonant.
BAE +, no added sounds heard.
CNS
GCS - 15/15
No focal neurological defects
All cranial neves are intact.
Higher mental functions intact
Power:-
Rt UL-5/5. Lt UL-5/5
Rt LL-5/5. Lt LL-5/5
Tone:-
Rt UL -N
Lt UL-N
Rt LL-N
Lt LL-N
Reflexes: Right Left.
Biceps. ++. ++
Triceps. ++ ++
Supinator. ++ ++
Knee. ++ ++
Ankle. ++ ++
Plantar: Flexion Flexion
ABDOMINAL EXAMINATION:-
Abdomen is soft and non tender
No organomegaly
Bowel sounds heard
No shifting dullness or fluid thrill
PROVISIONAL DIAGNOSIS : -
FEVER UNDER EVALUATION
ANEMIA of chronic disease?


Comments
Post a Comment