42 YEAR MALE WITH FEVER AND HEADACHE SINCE 20 DAYS
A 39 year old male ,farmer by occupation comes to casualty with complaint of fever ,headache and pain abdomen ,loss of appetite since 20 days.
Chief complaint
Patient complains of fever since 20 days,
headache since 20 days,
pain abdomen since 20 days
Loss of appetite since 15 days
History of presenting illness
Patient was apparently asymptomatic 20 days back then developed fever of insidious onset ,gradually progressive which increases during the night and relieves on taking medication,not associated with any rash.The day before the onset of fever patient was spraying pesticide in his field ,he supposedly wanted to finish two days of work in a single day and said that he was exposed to the fumes of the sprayer for a longer period of time since usual.
Pain abdomen is non radiating and not associated with nausea /vomiting ,not associated with diarrhoea
Headache is non radiating and mostly in the front and sides of the head .
Loss of appetite since 15 days
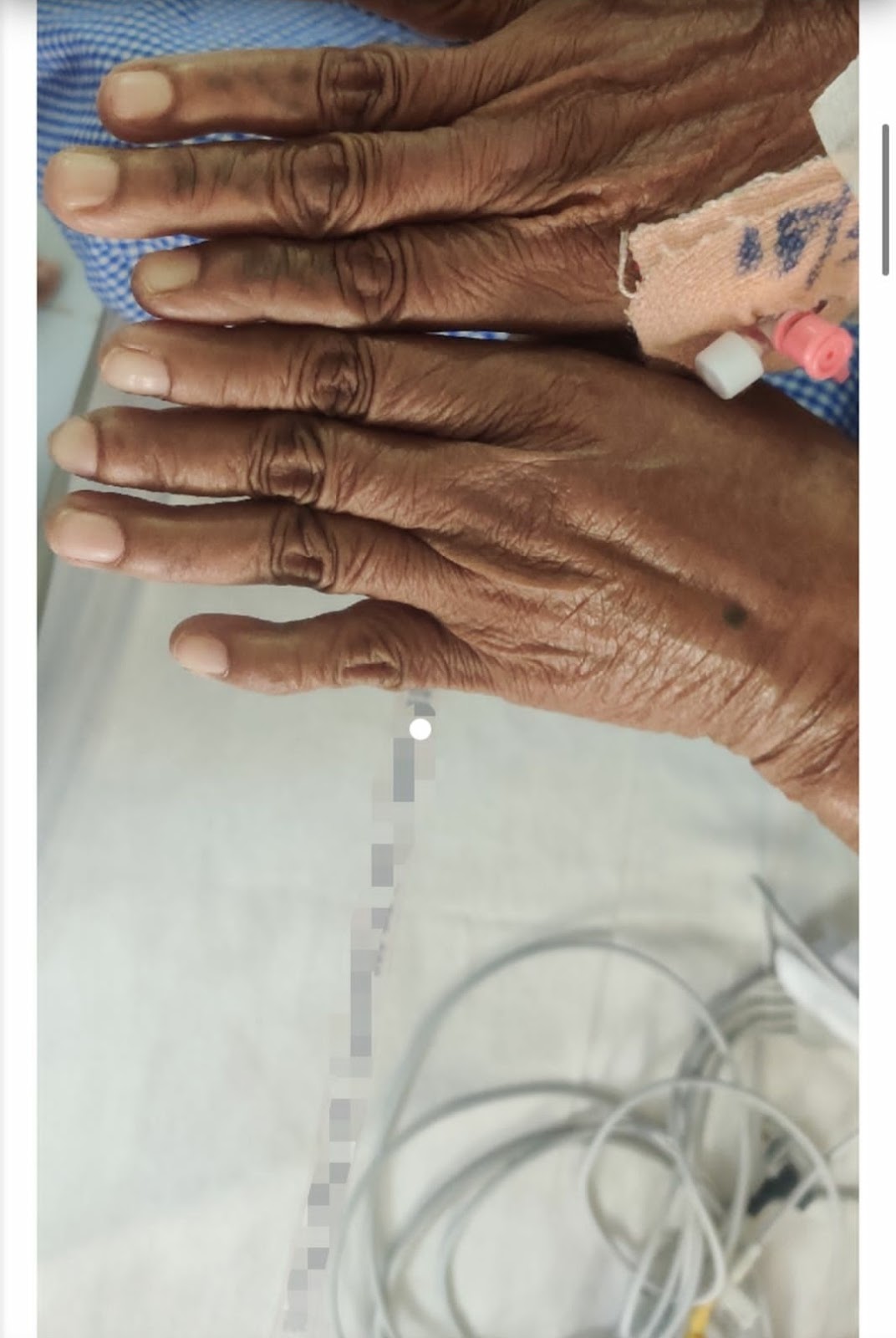
Patient noticed a scab on his left shoulder 5 days after admission to the hospital ,suspicion of an insect bite while he was asleep in his field 20 days ago
PAST HISTORY
Similar complaint of fever and pain abdomen 2 months ago received in 3 days on taking paracetemol tablets ,symptoms occurred after swimming in the local lake on the day before
Patient was also diagnosed with a stomach ulcer 5 months back ,the symptoms were releived on medication prescribed by a gastroenterologist at a local government hospital.No recurrent episodes since then.
Not a known case of hypertension/diabetes/thyroid /tuberculosis/epilepsy/asthma
PERSONAL HISTORY
Appetite is decreased
Mixed diet
Sleep is not adequate
Bowel and bladder movements are normal
No known allergies
Patient denies of use of tobacco
Patient consumes alcohol regularly ,toddy 1 litre every few days in the afternoon since the patient was 15 years old
FAMILY HISTORY
No relevant family history
No known cases of diabetes/hypertension/ tuberculosis/asthma/epilepsy/thyroid
PHYSICAL EXAMINATION
GENERAL
Patient is conscious ,coherent and cooperative
Patient is well oriented to time and place
Moderately built and moderately nourished
Pallor:absent
Icterus: absent
Clubbing:absent
Cyanosis:absent
Lymphadenopathy: absent
Edema: absent
VITALS
Temperature: afebrile
Pulse:99
Respiratory rate: 20bpm
Blood pressure: 110/80
SpO2 at room air: 99%
GRBS:115mg%
SYSTEMIC EXAMINATION
Cardiovascular system
s1 and s2 heard ,no murmurs
Respiratory system
Central position of trachea
Vesicular breath sounds
No wheeze,no dyspnea
Abdomen
Scaphoid shape
No tenderness
No palpable masses
No bowel sounds
PROVISIONAL DIAGNOSIS: viral pyrexia
FEVER CHARTING
1.Hemogram
Hemogram done on day of admission
PCV reduced
Decreased RBC count
MCHC reduced
Hemogram done 4 days after admissionPCV reduced
Decreased RBC count
MCHC reduced
Hemogram done 5 days after admission
PCV reduced
Decreased RBC count
MCHC reduced
2.urine examination
3.renal function tests
All renal function tests are normal
4.liver function tests
5.C-reactive protein
C- reactive protein is raised
6.Urine protein/creatinine ratio
7.Dengue NS1 antigen test
Dengue NS1 antigen test is negative
10. Test for HIV
HIV is negative
11.ultrasonography
Done on suspicion of a liver abscess
FINDINGS:
liver is normal
Pancreas is normal
Spleen not is normal
Right and left kidney are normal
No ascites
No lymphadenopathy
Normal echotexture
Diagnostic: rickketsial fever
TREATMENT
Normal saline 100 ml per hour continuously
Inj.Neomal 100 ml if temperature > 101.1 F
Inj.Pantop 40mg/IV OD
Inj.Zofer 4mg /IV TID
Tab.doxycycline 100 mg BD
Tab DOLO 650 mg TID
STRICT CHARTING
monitor vitals 4th hourly
















Comments
Post a Comment