65 year old male patient with pedal edema
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
A 65 year old male presented to OPD with cheif complaint of
1.pedal edema since 20 days
2.shortness of breath since 20 days
3. Cough with expectoration
HOPI
patient was apparently asymptomatic 20 years ago when he had an episode of acute left sided chest pain associated with chest pain for which he consulted a local physician and was prescribed medication (isosorbide dinitrate) ( suspected CAD) .
Since the last year year the patient has had bilateral pedal edema of pitting type till the knees on and off along with shortness of breath for 10 days .Patient has no associated history of chest pain,pain in the legs or fever .The patient consulted a local physician in lieu of these symptoms and was prescribed medication for the same.
Patient was also disturbed by the passing of his wife 1 year ago ,the event caused him extreme mental agony and led him to ignore his health and patient started smoking aggressively.
PAST HISTORY
Patient is a hypertensive diagnosed 1 year ago and is on treatment
Patient also has a history of CAD since 20 years and is on treatment (isosorbide treatment 10 mg)
Patient has no history of DM/THYROID/EPILEPSY/TUBERCULOSI-S
PERSONAL HISTORY
DIET: mixed
APPETITE normal
SLEEP: adequate
ADDICTION: chronic smoker since the laste 20 year , 1 pack since 40 years
BOWEL AND BLADDER: regular
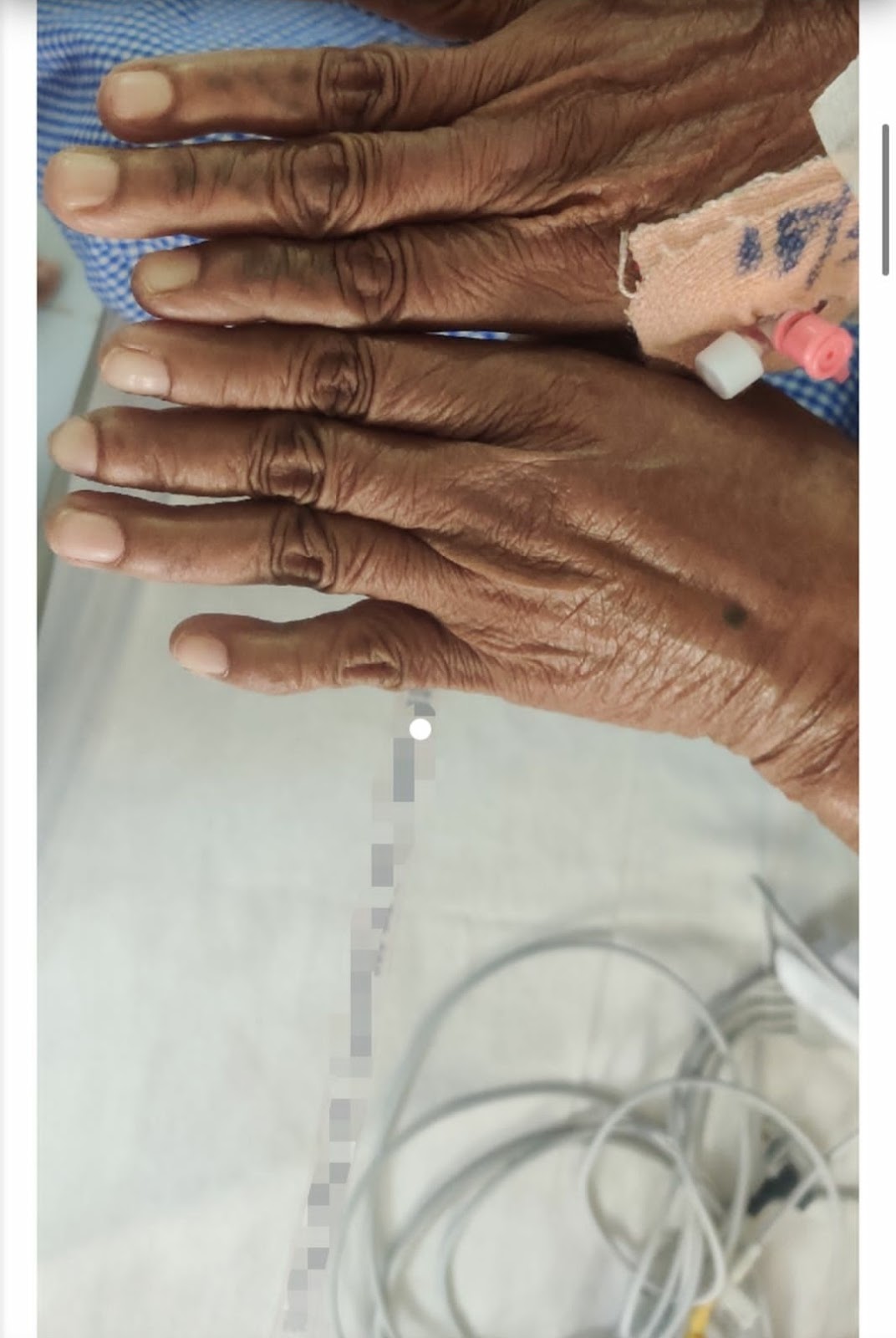
General examination
Pallor: absent
Icterus:absent
Clubbing: absent
Cyanosis: absent
Lymphadenopathy: absent
Edema: absent
Vitals:
Temp: afebrile on time of examination
BP 140/45
Heart rate 86 bpm
Resp Rate 24/min
Respiratory examination
Inspection : Chest bilaterally symmetrical
Palpation: Trachea central, chest expansion normal
Percussion: Resonant
Auscultation: B/l equal air entry, slight crepitations
CVS examination:
Inspection: No precordial buldge. Apical impulse visible.
No raised JVP ( intially present when presented to hospital , subsided post treatment.
Video:JVP
Palpation: Apical impulse, No palpebral pulsation.
thrill
Auscultation: S1 S2, No murmur
Abdominal examination:
Abdomen is soft and non tender
No organomegaly
No shifting dullness
No fluid thrill
Bowel sounds heard
Provisional diagnosis:
Cor pulmonale secondary to COPD ( smoking ?)
Investigation
2-d echo : DILATED RIGHT VENTRICLE AND ATRIUM
Chest x ray: BRONCHOVASCULAR MARKING ALONDISDE CARDIOMEGALY SUGGESTING CHRONIC LUNG DISEASE SUCH AND COPD
ECG












Comments
Post a Comment