80 year old female with SOB
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
80 year old female presented with
- Increase in Shortness of breath since 3 days
- Bilateral pedal edema since 3 days
- Generalized weakness since 20 days
- History of fall 20 days back
Patient was apparently asymptomatic 25 days back then she suffered trauma due to slipping in the bathroom, she fell in sitting position and complained of left hip pain.
She could walk normally for the next 4 days but later complained of left sided hip pain and was confined to her bed.
She developed of Shortness Of Breath which was insidious in onset. She had SOB grade 2 since 1 week which then progressed to grade 3/4 over the next few days on account of which was taken to a local hospital where she was put on Oxygen support after which her SOB improved
10 days back, She was unable to recognize her son in laws and had several episodes of irrelevant speech at inappropriate timings and a few episodes of fear. She was also unable to sleep at night ,instances of which still continue till date
4 days ago she complained of SOB grade 3/4 associated with bilateral swelling of the legs till the level of here ankle.
I/V/O these symptoms patient was taken to hospital and a CT scan was done, which didn’t reveal any abnormalities.
PAST HISTORY:
H/o COVID 19 infection in April 2021, her symptoms were cold, Shortness of breath and generalized weakness, for which she isolated at home and used medication for 1 week. All her symptoms improved but the weakness took 3 months to subside.
She was diagnosed with Hypertension 20 years back when she had an episode of giddiness associated with loss of consciousness, she received treatment for 3-4 days at the hospital.
She was also diagnosed with Diabetes Mellitus 13years back when she went for a regular check up.
Surgical history:
Underwent appendectomy 45 years back and hysterectomised 20 years back.
No history of blood transfusions.
No history of orthopnea/PND.
Personal history:
Diet: mixed
Sleep: disturbed, unable to sleep at night
Bowel and bladder movement: regular
Addictions: none
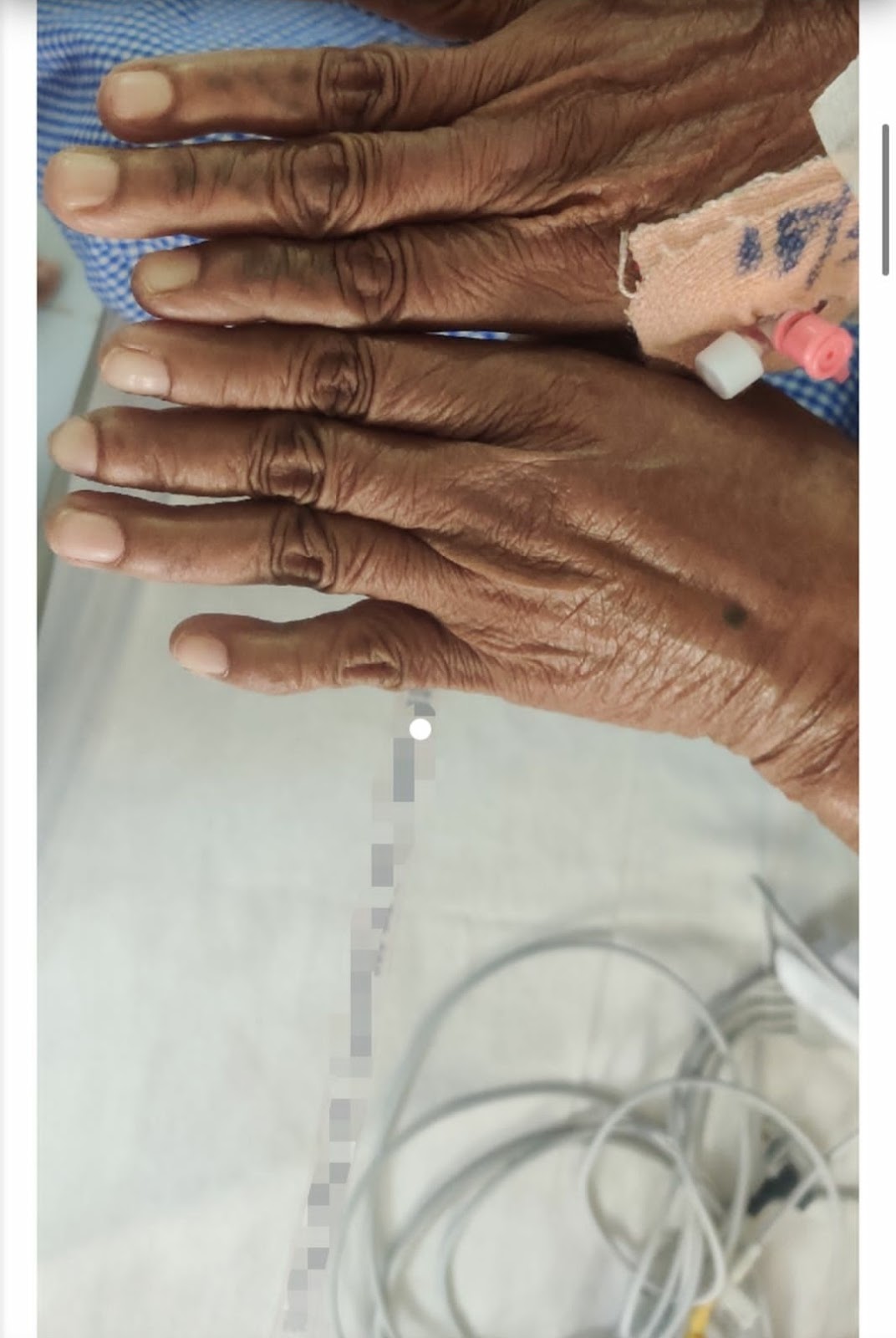
General examination:
Patient is conscious, coherent and cooperative.
She is oriented to place and person but not to time.
Pallor present.
No icterus, cyanosis, clubbing, lymphadenopathy.
B/L pedal edema of pitting type
Vitals on admission:
Temp: 98.6
PR: 90/min
BP: 120/70 mmHg
CVS: S1 S2 present
JVP raised
RS: BAE +
Decreased breath sounds on both side.
CNS: E4V5M6
P/A: soft, non tender
Investigations:
BGT: O positive
HEMOGRAM:
Hb: 8.3
TLC: 13,300
N/L/E/M: 79/11/4/6
Plt: 4.37 lakh
PCV: 24.9
MCH: 26.0
Serum Iron: 58
Retic count: 1.8%
Troponin I: negative
Serology: negative
RBS:189mg/dl
HbA1c: 6.9%
ESR: 25
CRP: Positive (2.4mg/dl)
LFT:
Tb: 0.69
DB: 0.20
AST: 798
ALT: 644
TP: 5.8
X- RAY OF CHEST ,HIP
Bat wing appearance indicating pleural effusion.
USG:
Diagnosis
RIGHT VENTRICULAR FAILURE WITH
PULMONARY ARTERIAL HYPERTENSION WITH ACUTE HEPATITIS
WITH DM & HTN
Treatment:
1.Tab. ECOSPORIN/AV 75/20 mg OD
2. Inj. MONOCEF 1gm IV BD (D2)
3. Inj. LASIX 20mg IV BD
4. GRBS 6th hourly
DISCUSSION
1) pathogenesis of right heart failure
2). Heart failure has been associated with an increased risk for hip fracture, and previous studies report a 6-20% prevalence of preoperative heart failure in hip fracture patients.
Reference:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3230699/#:~:text=Heart%20failure%20has%20been%20associated,failure%20in%20hip%20fracture%20patients.
3)HF is associated with ICF( impaired cognitive function) , manifested primarily as delirium in hospitalized patients, or as mild cognitive impairment or dementia in otherwise stable outpatients. This association is likely the result of shared risk factors, as well as perfusion and rheological abnormalities that occur in patients with HF. Evidence suggests that these abnormalities may be partially reversible with standard HF therapy.
Reference: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2684513/










Comments
Post a Comment