34 year old female with itching and red lesions ( CASE TAKEN IN MARCH)
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT."
34 year old female ,homemaker by occupation comes to casualty with complaint of fever ,shortness of breath and dry cough ,loss of appetite since 7 days.
Chief complaint
History of presenting illness
The patient was apparently asymptomatic 1 yr back when she developed b/l knee joint pain and itching in upper aspect of chest and neck.The pain was insidious in onset and gradually progressive and also associated with morning stiffness for which she was prescribed medication at a local hospital
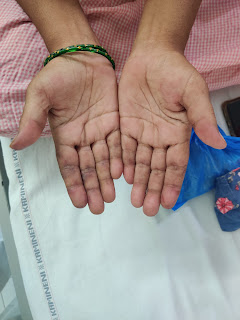
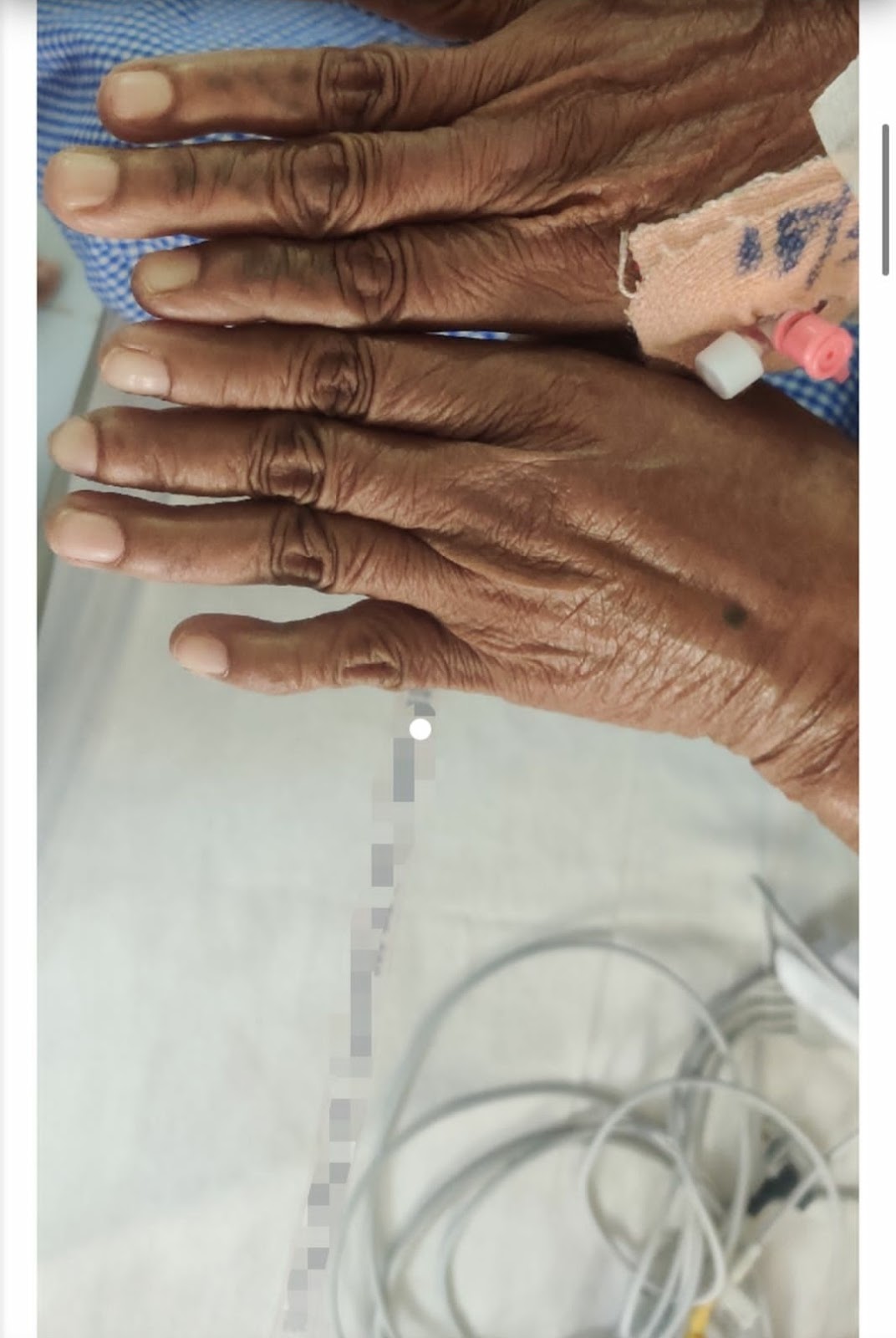
At the same time she had itching over neck and chest and hands the areas were covered with red lesions and later on turned black.
She also complained of generalized pain and muscle weakness of the proximal and distal(?) muscles since 1 yr
There was complaint of b/l pedal edema and sob(grade 3) since 6 to 7 months which was gradually progressing to the present state.
C/o vaginal discharge 8 to 9 months back which was curdy white and later changed to watery and clear in nature.
C/o oral and genital ulcers since 1 yr
About 2 months back she came to the hospital with the above mentioned complaints and was diagnosed with DERMATOMYOSISTIS with vaginal candidiasis .
Patient was referred to other health centre for muscle biopsy.
Her ANA immunofluoroscence showed homogeneous pattern.Intensity 4+ associated antigens involved-ds DNA,histones.
HRCT was done -
IMPRESSION: Few patchy areas of ground glass opacities in peri bronchovascular distribution-s/o pneumonitis (Corads-4)
About 5 to 6 days back she developed high grade fever associated with chills and rigors which is continuous and relieves only on taking medication. She had cough from 5 to 6 days with sputum which is more during night time. She is experiencing shortness of breath even at rest (grade 4) since 5 days. There is bilateral pedal edema involving till below the knee.
When she went to the nearby facility they told her that it might be pneumonia and gave some medications but it did not help.
PAST HISTORY
No history of hypertension/diabetes/thyroid /tuberculosis/epilepsy/asthma
PERSONAL HISTORY
Appetite is decreased
Mixed diet
Sleep is not adequate
Bowel and bladder movements are normal
No known allergies
Patient denies of use of tobacco and alcohol
FAMILY HISTORY
No relevant family history
PHYSICAL EXAMINATION
GENERAL examination
Patient is conscious ,coherent and cooperative
Patient is well oriented to time and place
Moderately built and moderately nourished
Pallor:absent
Icterus: absent
Clubbing:absent
Cyanosis:absent
Lymphadenopathy: absent
Pedal Edema: present
VITALS
Temperature: 99
Pulse:73
Respiratory rate: 20bpm
Blood pressure: 150/100
SpO2 at room air: 99%
SYSTEMIC EXAMINATION
Cardiovascular system
s1 and s2 heard ,no murmurs
Respiratory system
Central position of trachea
Vesicular breath sounds
No wheeze,no dyspnea
Abdomen
Scaphoid shape
No tenderness
No palpable masses
No bowel sound
Investigation
Provisional diagnosis
Dermatomyositis ( need to rule out intersitial lung disease)
Day 2-3
Patient had a decrease in cough and shortness of breath from grade 4 to grade 2
Fever charting showed no spikes on these days
Treatment regimen unchanged
Day-4
Patient condition detiorated from 9:00 pm when she devloped cough along with sputum and sob grade 4 and fever.
Fever charting showed a fever spike
Patient shifted to ICU and put on oxygen support
DISCUSSIONS
1)Cause of dermatomyositis:
MDA-5, formerly known as CADM-140, is a RIG-I-like pattern recognition receptor of the innate immune system.1, 3 It identifies viral dsRNA within the cytosol, the fluid portion of cytoplasm, and prompts the manufacture of type 1 interferons, which ultimately provoke apoptosis of the infected cells.3 The precise roles MDA-5 and the anti-MDA-5 autoantibody play in dermatomyositis are not completely understood. In brief, it is thought that in some patients, production of anti-MDA-5 autoantibodies occurs during viral infections of the skin and lung epithelium. Their formation is triggered by the release of fragments of MDA-5 after its proteolysis within infected cells. These autoantibodies are believed to injure endothelial cells and other tissues.2
The papules that form in patients with dermatomyositis are often painful and ulcerated, and they are usually located on the palmar surface of the metacarpophalangeal and interphalangeal joints.4, 5 This finding and others, including ulceration, livedoid appearance, tender gums, and mechanic's hands, are likely explained by vasculopathy.3, 4, 5 Nonscarring alopecia and panniculitis can also occur.
2)RELATION TO ILD:
Learning points:
**1.Immune pneumonia in DERMATOMYOSITIS patients:.*
Involvement of immune mechanisms is supported by the presence of T cells, macrophages in muscle tissue, by the presence of autoantibodies and by HLA-DR being a strong genetic risk factor
A newly identified T cell subset, CD28null T cells, may have cytotoxic effects in the CD4+ and CD8+ T cell phenotype. These cells are apoptosis resistant and may contribute to treatment resistance.
The interstitial lung diseases characterized by inflammation, fibrosis involving the lung parenchyma and a most common complication of DERMATOMYOSITIS.The target of injury includes the critical alveolar-capillary interface responsible for gas exchange.








Comments
Post a Comment