57 year old female with diarrhea
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
57 year old female presented to opd with cheif complaints of
1.fever since 2 days
2.loose stools since 2 days
3.generalized body weakness since 2 days
HOPI
Patient was apparently asymptomatic 2 days back then she had 5 episodes of diarrhea along with 1 fever spike and pain abdomen , the pain abdomen was diffuse the following day she had 2 episodes of vomiting and 4 episodes of diarrhea.
History of consumption of outside food 2 days ago
Patient has no complaint of chest pain , palpitations,headache .
The next day she had 8 episodes of diarrhea ,no complaint of pain abdomen
PAST HISTORY
Patient has hypertension since the last two years
Patient has no history of DM/THYROID/EPILEPSY/
TUBERCULOSIS/ASTHMA
DAILY ROUTINE
Patient wakes up at around 6 in the morning and helps with household chores . patient has breakfast around 8 am and usually consumes fruit. Patient has lunch at around 1:30 pm and consumes curd rice along with a banana ,due to digestive issues the patient usually avoids spicy food.
Dinner is had around 8pm and consists the same as lunch.patient goes to bed at around 10 pm.
Patient stays at home for most of day as she is retired
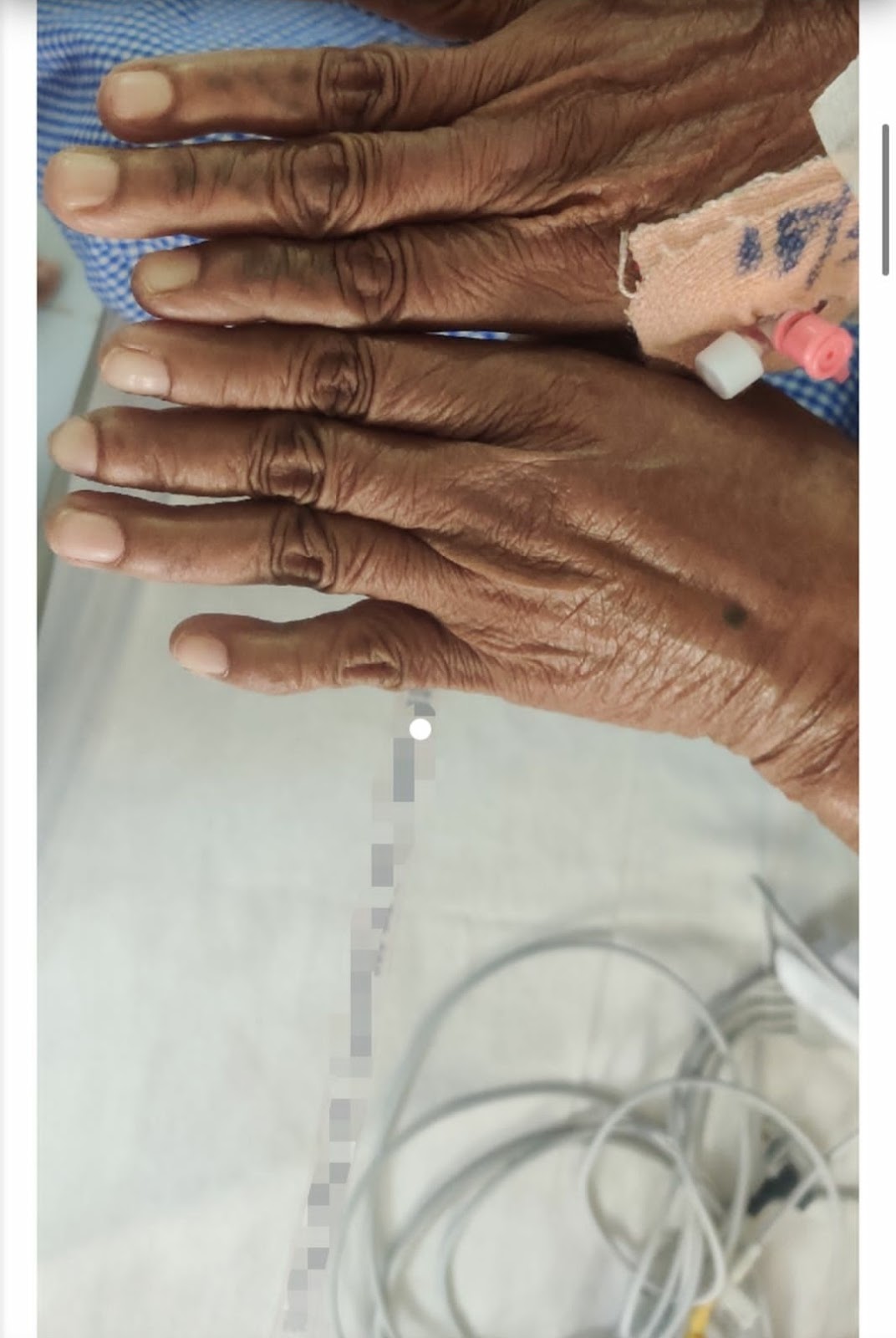
General examination
Pallor: absent
Icterus:absent
Clubbing: absent
Cyanosis: absent
Lymphadenopathy: absent
Edema: absent
Vitals:
Temp: afebrile on time of examination
BP 140/45
Heart rate 110 bpm
Resp Rate 16/min
Abdominal examination:
Abdomen is soft and non tender
No organomegaly
No shifting dullness
No fluid thrill
Bowel sounds heard
Respiratory examination
I: Chest bilaterally symmetrical, all quadrants
moves equally with respiration
P: Trachea central, chest expansion normal
P: Resonant
A: B/l equal air entry, no added sounds heard
CVS examination:
I: No precordial buldge. Apical impulse
visible, Venous prominence
P: Apical impulse, No palpebral pulsation.
thrill
A: S1 S2, No murmur
INVESTIGATION
2-D echo
Ultrasound
Differential diagnosis
Acute gastroenteritis
(Greenish stool could indicate that you have a bacterial infection (salmonella or E. coli, for example), viral infection (norovirus) or a parasite (Giardia) causing a rapid transit “gush” of unabsorbed bile)












Comments
Post a Comment